
- For Public
- For Patients
- Healthcare Professionals
- For Partners
- General Practitioners
- Community Partners
- Workplaces
- Schools
- Research & Innovation
- Careers
- Giving
- About Us
- I Want To
Overview
What are the diabetes-related foot deformities?

Foot deformities—abnormal changes in the shape of the toes, arches, or bottoms of the feet—increase your risk of diabetic foot complications such as ulcers, infections, and pain.
These deformities can range from claw toe and high arches to a severely deformed rocker-bottom foot (Charcot foot).
Causes
Poorly controlled blood sugar can damage the nerves in the feet and weaken foot muscles, which can lead to foot deformities.
A high-arched foot (pes cavus) and clawing of the toes in people with diabetes develop as a result of weakened foot muscles. This occurs because diabetes affects the nerves that supply sensation and movement to the foot muscles.

Charcot foot is a rare but severe condition affecting the foot and ankle in people with diabetic neuropathy. Individuals may not recall any significant trauma and often continue walking on the affected foot because nerve damage prevents them from feeling pain. Repeated pressure can further damage bones and joints, ultimately altering the foot’s shape and structure.
ATTENTION! Early detection of Charcot foot is crucial. Joint collapse leads to irreversible changes in foot shape and structure. Without reconstructive surgery, the foot will not return to normal, making it difficult to find shoes that fit. High-pressure areas may develop thickened skin (calluses) that can break down into ulcers and become infected.
What are the symptoms?

Abnormal shapes in foot and toes.

Early signs of an active Charcot foot include swelling and warmth in the foot or ankle. Pain or redness may also occur.

The person may not feel pain, or may feel less pain than someone without nerve damage.

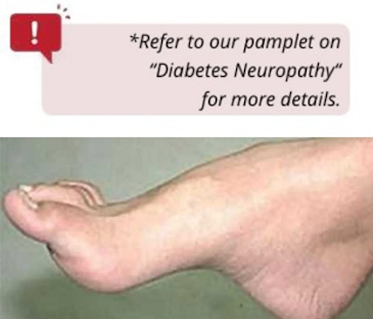
Charcot foot often leads to a rocker-bottom deformity, usually due to delayed diagnosis and management.

Some individuals may develop foot wounds (ulcers) or infections.
Prevention

Controlling your blood sugar is a key step in preventing Charcot foot by reducing your risk of developing diabetic neuropathy..

It is essential to check your feet at least once daily.

Examine your feet daily for cuts, sores, injuries, or changes in the shape of your feet or toes.

Wear properly fitted shoes. If you have diabetes and significant foot deformity (such as Charcot foot), your podiatrist may recommend custom footwear and/or insoles.

Always check the inside of your shoes for loose objects that could cause injury before wearing them.
Related Articles
Detection & Treatment

If you have an active Charcot foot, your podiatrist or orthopedic surgeon may recommend wearing a plaster cast or protective walker boot.

You may also be advised to use crutches or a wheelchair to minimize weight-bearing on the affected foot.
This recovery process may take months. It is important to work closely with your podiatrist, orthopedic surgeon, or specialists in the multi-disciplinary foot clinic.

It is crucial to wear the protective boot or plaster cast prescribed by your podiatrist to prevent further changes in your foot’s shape. Crutches, a knee walker, or a wheelchair may also be prescribed to keep weight off the affected foot.

You may be advised to minimize walking while you have a below-knee cast.

After the cast is removed, you may be advised to use custom insoles or footwear to ensure a proper fit and relieve pressure points.

Surgery may be recommended by your orthopedic specialist if you have serious ankle or foot deformities that are unstable or at risk of developing a foot ulcer.

Keep your diabetes, high blood pressure, weight, and cholesterol under control.

Quit smoking.
Care Management
Specialties & Services